 What’s it like in our journey with Frontotemporal Degeneration currently? Most of Chuck’s symptoms from FTD come from his loss of what is known as “executive function”. It was quite difficult for me to understand what I was seeing when this started and to describe this to his doctors. Once I understood executive function, and dysfunction, things became so clear.
What’s it like in our journey with Frontotemporal Degeneration currently? Most of Chuck’s symptoms from FTD come from his loss of what is known as “executive function”. It was quite difficult for me to understand what I was seeing when this started and to describe this to his doctors. Once I understood executive function, and dysfunction, things became so clear.
When we think about cognitive abilities and a dementia diagnosis, we often focus on memory. Forgetting people, places, things, losing things,etc. However, another critical aspect of our brain’s work is executive function. This term describes an essential set of mental skills that enable us to plan, organize, manage time, and make decisions. These skills help us navigate daily life, handle challenges, and adapt to new situations. Once I understood what executive function was, so much made sense in what I was seeing in Chuck that was so perplexing.
What happens when someone begins to lose executive function? Recognizing the symptoms of executive dysfunction was crucial for understanding changes in Chuck’s behavior and for responding appropriately.
I will explain what executive function is, and try to help others in understanding some of what we experience currently as we navigate Chuck’s diagnosis of FTD.
Executive function is like the control center of the brain. It comprises a group of mental skills that allow us to regulate our thoughts, emotions, and actions. Generally, executive function includes:
1. Planning and Organizing: The ability to set goals, plan steps to achieve them, and organize information and tasks.
2. Time Management: Being able to prioritize activities, keep track of time, and follow a schedule.
3. Problem-Solving and Decision-Making: Identifying a problem, evaluating potential solutions, and making an informed decision.
4. Flexibility and Adaptability: Adjusting to new information or changes in circumstances.
5. Self-Control: Managing impulses and maintaining focus on a task.
6. Working Memory: Holding and using information briefly for performing tasks or responding to demands.
These abilities are interconnected, allowing us to carry out everything from routine chores to complex projects. However, when these skills start to decline, it’s known as executive dysfunction.
Several factors can impact executive function, and these vary by age, health, and environment. Some common causes include:
• Neurological Conditions: Frontotemporal dementia (in our case!), Alzheimer’s disease, Parkinson’s disease, and traumatic brain injuries can impair executive function.
• Mental Health Disorders: Conditions such as depression, anxiety, and attention-deficit/hyperactivity disorder (ADHD) are often linked to executive function challenges.
• Aging: While some cognitive decline is normal with aging, noticeable executive function loss isn’t a given for everyone.
• Stress and Overwhelm: High-stress levels over time can reduce our ability to focus and problem-solve, mimicking some symptoms of executive dysfunction.
Understanding the cause can help tailor approaches to managing symptoms and making life easier for those experiencing them.
Loss of executive function may appear gradually, and symptoms vary depending on the individual and the underlying cause. Here are some common signs to watch for:
1. Difficulty Planning and Organizing
People with executive dysfunction may struggle to put a plan together or remember steps needed to complete a task. Something that once felt automatic, like preparing a meal or paying bills, might now feel overwhelming. One of the things I noticed in this category was that he was unable to carry out the necessary steps to grill hamburgers. It sounds simple, but this involves steps that were difficult to sequence and complete
2. Poor Time Management and Awareness
They might have difficulty estimating how long tasks will take or frequently run late because they can’t track time effectively. They might also miss deadlines or appointments because organizing their time has become challenging. One example for us in this category is not realizing it’s time for a meal and initiating grabbing his lunch. He also has no concept of getting ready and out the door to be somewhere at a certain time. These require assistance from me to keep him on task and moving forward.
3. Struggles with Decision-Making
Everyday decisions, like what to eat or what to wear, can become confusing or paralyzing. Faced with multiple choices, people may feel overwhelmed and unable to choose. This is why Chuck may come downstairs wearing what he had on yesterday. It must have been a good choice then, so it works again today.
4. Reduced Problem-Solving Abilities
Problem-solving becomes challenging. In situations where they would have been able to calmly assess and act, they might now struggle, repeat mistakes, or abandon the task altogether. He’s no longer able to help with the household decision making. Rather, he is like a dependent in the home that requires help with any problem solving.
5. Rigid Thinking and Difficulty Adapting
Loss of flexibility is common in executive dysfunction. New situations or changes to routine can become stressful, and they may have trouble adapting, preferring to stick rigidly to habits or routines. We see this daily and navigate changes slowly.
6. Impulsivity and Lack of Self-Control
Managing impulses becomes harder. This could manifest in things like saying things out of turn, making inappropriate comments, or reacting emotionally in situations that require patience. Oh, the things I’ve heard him say, usually just to me currently, but that day will come when others will hear the comments. One thing I’ve noticed with his disinhibition publicly is that he’s usually trying to be helpful with others, such as approaching a mother in a parking lot to help load her groceries.
7. Poor Working Memory
Working memory issues make it hard to keep multiple pieces of information in mind. For example, they may lose track of a conversation or forget what they were about to do. Chuck will head off to take the trash out when I ask but forget to close a door, forget to bring a trash bag back or not complete the task altogether. If I ask him to turn a light out, he says he will but then it doesn’t happen. I have found that it’s best to accept what happens or doesn’t, and to pick up where he drops off or ask him again.
Executive dysfunction can be challenging, but there are supportive strategies to manage symptoms. These may include:
• Creating Routines and Using Tools: Simplify tasks by using checklists, setting reminders on devices, and developing consistent daily routines. For his medicine, Alexa sounds a reminder twice a day. If he doesn’t respond by taking his meds right away, then the moment is lost. So while helpful most days, we cannot rely completely that this will get the job done.
• Breaking Down Tasks: For someone experiencing executive dysfunction, breaking larger tasks into small, manageable steps can ease frustration. Chuck is great at getting the dishwasher unloaded if I ask, but often can’t get the dishes in the correct spots. I’ll take it.
• Allowing Extra Time: Providing plenty of time for tasks can reduce stress, especially in timed situations. Gone are the days when he could be ready and out the door in 15 minutes. He requires assistance with staying on task for something like getting ready to leave the house or else I find him wandered off to something else. I have to allow enough time myself to help ensure he’s moving forward.
• Encouraging Physical and Mental Exercises: Activities that stimulate the brain and body can support mental health and executive functioning. Thank goodness for our dog that pesters him for daily walks. Chuck has been slowing down lately and doing less, but every little bit helps. He enjoys reading the newspaper and will read a copy over and over and over. He also loves to read things online.
• Seeking Professional Guidance: Occupational therapists, psychologists, and neuropsychologists can offer strategies and coping mechanisms tailored to the individual. We have sought input from his doctors as well as palliative care.
Symptoms may not always be easy to manage, but support can make a significant difference. Practicing patience and maintaining open communication are key. Not always easy! Understanding that it’s the condition, not the person, at the heart of these behaviors can also make the journey smoother.
With understanding, practical strategies, and assistance, people experiencing executive dysfunction can navigate daily life. It definitely requires patience and assistance from the care partner. I’m learning new strategies and working on this daily. What I have learned is that frontotemporal degeneration presents differently in every person. So far, for us, loss of executive function and especially the working memory seem to be the biggest challenges.
Chuck can no longer navigate daily life without input, direction, and assistance. He cannot be “trusted” to take his meds, complete personal care, get his meals, or flow through with the tasks he needs to do. He can’t read a menu and remember what he wanted to order. And so much more. So, as his wife and life partner I will help him. His children help him. It is certainly not easy. No longer having someone to help navigate the challenges of life with, but having to help them with the challenges, can be daunting at times. Having compassion for the situation is key.
Being empathetic to the situation can go a long way in understanding those with FTD and their care partners.
#endFTD #AFTDAmbassador #supportcarepartners #NationalCaregiverMonth

 One of the hardest parts of life with frontotemporal dementia (FTD) isn’t always the big changes — it’s the quiet, everyday moments that remind you how much this disease shifts reality for both of you.
One of the hardest parts of life with frontotemporal dementia (FTD) isn’t always the big changes — it’s the quiet, everyday moments that remind you how much this disease shifts reality for both of you.


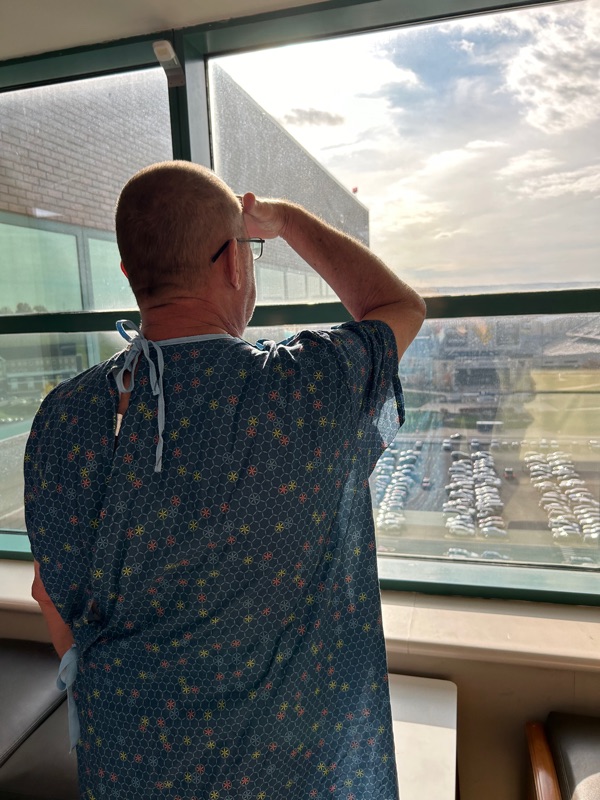 I want to share an update on Chuck’s health. Saturday night he had a stroke. He had a sudden onset of slurred speech and left sided weakness/paralysis. A trip to the hospital, a clot buster drug and a flight to Ruby in Morgantown ensued.
I want to share an update on Chuck’s health. Saturday night he had a stroke. He had a sudden onset of slurred speech and left sided weakness/paralysis. A trip to the hospital, a clot buster drug and a flight to Ruby in Morgantown ensued.  What’s it like in our journey with Frontotemporal Degeneration currently? Most of Chuck’s symptoms from FTD come from his loss of what is known as “executive function”. It was quite difficult for me to understand what I was seeing when this started and to describe this to his doctors. Once I understood executive function, and
What’s it like in our journey with Frontotemporal Degeneration currently? Most of Chuck’s symptoms from FTD come from his loss of what is known as “executive function”. It was quite difficult for me to understand what I was seeing when this started and to describe this to his doctors. Once I understood executive function, and